CURE FAQs: Frequently Asked Questions
Answers to commonly asked arterial and metabolic disease questions.
Categories
Click on one of the categories below or type a keyword into the search bar to get started.
Recent FAQs
What is visceral fat and how do I reduce it?
There are two types of fat that our body stores: subcutaneous fat and visceral fat. Subcutaneous fat is stored just under the skin. We can feel it in our arms, legs, and hips. Think of it as the fat that you are able to pinch with your fingers…
There are two types of fat that our body stores: subcutaneous fat and visceral fat.
Subcutaneous fat is stored just under the skin. We can feel it in our arms, legs, and hips. Think of it as the fat that you are able to pinch with your fingers.
Visceral fat, or visceral adipose tissue, is the fat that is stored inside the body cavity and wraps itself around and infiltrates our internal organs, such as the heart, liver, or intestines. This fat is metabolically active and functions as if you had another organ in your body which produces negative hormonal effects. We call it “angry” or “inflammatory” fat.
Why is visceral fat dangerous?
Visceral fat is also referred to as “active” or “inflammatory” fat because it produces substances that contribute to insulin resistance, leading to Type 2 Diabetes. Insulin resistance is the prediabetic state where your body is losing its ability to properly balance insulin and regulate blood glucose.
Visceral fat secretes a protein called retinol-binding protein 4 (RBP4) that increases insulin resistance in the body. It also releases inflammatory substances called cytokines, which leads to chronic inflammation.
High levels of visceral fat are associated with increased risk for:
Type 2 Diabetes
Heart disease
Breast cancer
Colorectal cancer
Alzheimer’s disease
Nonalcoholic fatty liver disease (NAFLD)
It is very difficult to be healthy with high amounts of visceral fat. Lowering visceral fat eliminates a major driver of chronic diseases.
What are the sources of visceral fat?
The root causes of visceral fat are refined carbohydrates, processed foods, and artificial sweeteners ingested without periods of fasting. This type of diet is typical in Western cultures. In order to eliminate visceral fat, the secret is to minimize the five S’s: Sweets, Starch, Snacks, Seed oils, and Sitting.
How do you test for visceral fat?
There are many ways to estimate your visceral fat. MRI, DEXA, and CT scans are accurate but costly and inconvenient. A cheaper way to estimate visceral fat is to measure your waistline. A healthy waistline in women is typically 35” or lower, and 40” or lower for men. However, these measurements are prone to variability. They are inexpensive, but not precise.
At the CURECenter, we have a simple, non-invasive, and cost-effective way to measure and monitor visceral fat. We use the InBody 570 analyzer to obtain accurate body composition data on our patients repeatedly over time. This data allows us to monitor not only visceral fat, but percent body fat, skeletal muscle mass, and hydration levels. This information is crucial in monitoring the benefit of our treatment and demonstrating optimal results. The InBody data goes far beyond the scale and helps us provide motivation for ongoing lifestyle improvements.
Body composition tests using the InBody 570 only take a few minutes and are completely painless and non-invasive. The process is similar to stepping on a scale - only this machine measures much more than your average at-home device. If you have a pacemaker or defibrillator, or you are pregnant, we don’t use the InBody, even though the risk is not high.
How do I eliminate visceral fat?
Reduce your sugar intake, especially sugary drinks, refined white carbohydrates, and processed foods.
Avoid artificial sweeteners. They raise insulin in the same way as sugar, even though they are lower in calories. They also perpetuate cravings for real sugar by feeding your sweet tooth, like a “gateway” drug.
Restrict eating to a window of time (ideally 6-8 hours) and devote time every day to fasting (drinking only water or non-sugary drinks). At least 16 hours of fasting, including sleep, is a goal we promote to our patients. We call it “window feeding.”
Exercise as much as you can most days.
Eat a low-glycemic diet. Low-glycemic foods consist of green vegetables, whole fruits (in moderation), beans, and lentils.
Get a good night’s sleep. Too little sleep or too much sleep on a regular basis can lead to more visceral fat storage.
Manage stress. Mindfulness practices like prayer, meditation, or yoga can help manage your body’s stress response and lower cortisol levels.
Limit alcohol. When your liver is processing alcohol, it is not processing fat.
Quit smoking. Tobacco use can negatively affect your ability to deal with glucose and increase insulin resistance.
Targeted supplements and medications can improve insulin sensitivity for some individuals with stubborn visceral fat.
What is Insulin Resistance? Can it be reversed?
Insulin resistance occurs when the cells of the muscles, fat, and liver become insensitive or resistant to insulin, causing the body to produce higher insulin levels to compensate…
Insulin resistance occurs when the cells of the muscles, fat, and liver become insensitive or resistant to insulin. This causes the body to produce higher insulin levels in response to glucose intake to achieve the primary goal: Optimize blood glucose and its utilization as fuel. This state of hyperinsulinemia is highly inflammatory for your entire body, especially your arteries and nerves. Eventually insulin production fails and blood sugar levels begin to rise. It is at this point the patient is diagnosed with diabetes based on elevated blood glucose/”sugar”, the final stage of "diabesity."
However, even thin, lean people can be insulin resistant, especially if muscle mass is low (sarcopenia) relative to body fat, especially visceral fat. This is especially common for women after menopause.
Insulin resistance is so common that we should assume its presence till proven absent. Why is it so common to be called a “feature” rather than a “bug”? Why wouldn’t evolutionary pressures get rid of it? The answer: It is a benefit to the hunter gatherer lifestyle. It is not well suited for our current cultural habits of “grazing” constantly on sweets, starches and highly processed snacking. And, it doesn’t cause death prior to reproduction.
The answer: Eat like a hunter gatherer! Eat within a short time window (6 hours is ideal) and eat lots of vegetables, a little fruit (sugary!), meat/protein and good fat (olive, coconut or avocado oil, seeds, nuts).
What is Diabesity?
Diabesity is the spectrum of adverse health effects of diabetes and obesity. It is the result of a modern environment of processed food loaded with sweets and starches consumed throughout the day.
Before rising glucose levels are detected, the higher insulin levels (caused by insulin resistance) raise blood pressure and create inflammation that contributes to arterial injury. We call this injury and the resulting inflammation and scarring atherosclerosis. It can also lead to diabetes, dementia (Type 3 Diabetes?) erectile dysfunction, and depression. Risk of heart attack, stroke, and dementia also increase.
We develop "tolerance" to the toxic effects of sweets and insulin. This leads us to crave more sweets, driving our insulin levels higher, and can lead to early death and disability if unrecognized and untreated.
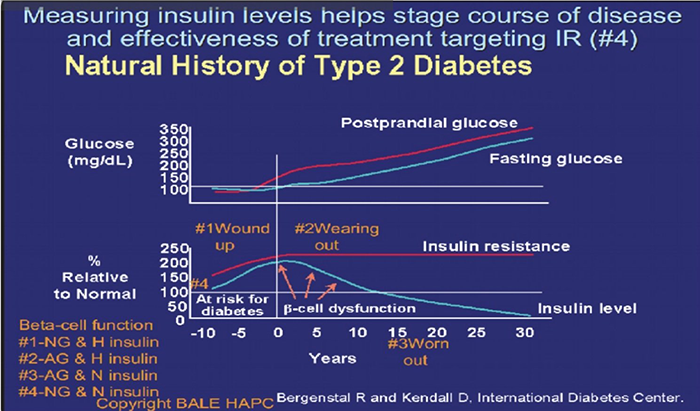
Image Source: International Diabetes Center
This graph illustrates the relationship between insulin resistance, rising insulin levels, and blood glucose levels associated with the progression from insulin resistance (“pre” prediabetes, prediabetes to Type 2 Diabetes. It should be labeled "The Natural History of "Diabesity."
What are some indicators of Insulin Resistance/Diabesity?
Some indicators of insulin resistance include (but are not limited to):
Increased waist size
Elevated visceral fat
High blood pressure
Elevated blood sugar
High triglycerides
Low HDL cholesterol (Metabolic syndrome)
Small dense LDL predominance (Pattern B)
Heart attack or stroke
Gestational diabetes
Polycystic Ovary Syndrome
Erectile Dysfunction
Ananthosis Nigricans
Periodontal disease
How do we identify Insulin Resistance/Diabesity?
The gold standard identifier of insulin resistance includes a two hour oral glucose tolerance test with simultaneous insulin levels. During this test, your blood is drawn before and after drinking a sugary liquid to see how your body responds. Measuring against certain high benchmarks define diabetes and prediabetes. Normal glucose (blood sugar) levels should be below 125 after one hour of this test and 120 after two hours.
Fasting glucose levels above 90 and HbA1c above 5.0 should raise concerns about insulin resistance until other measures are used to rule it out.
Other measures used to identify insulin resistance include: high triglycerides, low high-density lipoprotein (HDL), small and dense low-density lipoprotein (LDL), hypertension, non-alcoholic fatty liver disease (NAFLD), and “idiopathic” neuropathy. Insulin levels outside the context of response to standardized glucose intake or infusion are not helpful. Normal fasting insulin does not exclude insulin resistance or disprove and elevated levels tell us no more than other evidence already cited and generally availalable
At the CURECenter, we perform body composition analyses on all of our patients to help identify insulin resistance/diabesity. Elevated visceral fat (which correlates with percent body fat) can be detected in a few minutes, revealing some of the earliest evidence.
Visceral fat can be hard to identify without a body composition analysis, as one may appear “thin” on the outside, but still have high levels of visceral fat. These healthy looking individuals have low muscle mass, known as sarcopenia. This occurs especially in women after they experience menopause, especially if they avoid resistance exercises.
New options for continuous glucose monitoring, like Stelo make continuous glucose monitoring available without a prescription at affordable pricing for the masses. Stelo is even available on Amazon. The feedback from seeing the actual real time impact of food choices and other behavior, make this perhaps the most powerful tool in our battle against cardiometabolic disease. It confirms diagnosis, but more importantly offers individualized feedback about foods that should be avoided and choices that are safer to guide choices.
How do we reverse Insulin Resistance/Diabesity?
Dietary Changes: First, cut out sweets, starches, and snacks from your diet. Excess sugar in your daily diet is stored as fat, worsening insulin resistance. Avoid sugar, artificial sweeteners (they raise insulin and enhance cravings), processed foods, and bread, pasta, potatoes, and rice. These all raise insulin levels (even in the absence of high amounts of calories) and perpetuate cravings for sweets. These cravings are a form of addiction, much like addictions to drugs and alcohol.
In order to effectively reverse insulin resistance/diabesity, be sure to eat more vegetables, protein, and good fats (from sources such as olive oil, coconut oil, nuts, seeds, and fish).
Although fruit contains important vitamins, eat it in moderation. Fruit is higher in sugar (especially if dried or juiced) than vegetables. Eat whole fruit in limited amounts to ensure healthy glucose levels. Berries are the best. Apples, pears and other fibrous foods slow glucose absorption. Bananas and grapes are like candy bars and M&Ms!
Exercise: Get off the couch. A sedentary lifestyle is a recipe for all types of chronic disease. While nearly all types of physical activity can be beneficial, we recommend high intensity interval training and a focus on building muscle through resistance training in addition to aerobic/cardio exercise.
Restricted Feeding/Fasting: At the CureCenter, we see the best results in individuals who restrict their good food intake to an 6-8 hour window each day. In the other 16 hours of the day, drink only water or unsweetened beverages.
For additional information about healthy fasting, we recommend resources created by Dr. Jason Fung, including his books, “The Obesity Code,” and “The Diabetes Code,” blog (The Fasting Method), and YouTube channel.
Proper Amounts of Sleep: Poor amount and quality of sleep has been linked to higher levels of insulin resistance. Be sure to get proper amounts of sleep each night. More is generally better. Very few of us get enough sleep. It is rare to get too much sleep in the absence of sleep apnea.
Manage Stress: High levels of stress and associated high cortisol have also been linked to insulin resistance. Although it’s not always easy, try to find ways to relieve stress to reduce cortisol levels, which raise glucose and insulin. Exercise is a proven and healthy way to reduce stress. So get off the couch and go outdoors or to the gym. Mindfulness practices such as meditation, prayer, or yoga can also help to manage stress.
Measure Your Results: When you first start on your journey to reverse resistance to insulin, it’s best to measure your results every 1-2 weeks by taking a body composition test (these can be done at the CureCenter office). When you’ve met your goal, continue to test every 1-2 months to ensure you are staying on track. Staying accountable is key. Seeing improvement perpetuates the process.
Wear and pay attention to the results of a continuous glucose monitor for at least 2 weeks to identify threats and avoid them. For those who need the extra discipline and monitoring, doing so more often can help resist the influence of our pervasive and powerful harmful processed food culture.
We call it M&M’s (the healthy kind): Measure, Motivate, and Maintain Momentum.
Supplements and Medication (if goals not achieved by lifestyle changes alone ): Sometimes, insulin resistance is so stubborn that a healthy diet and exercise do not achieve the reduction in fat that one may expect. This can be due to an incomplete commitment to carbohydrate restriction or insufficient patience. We cannot out-prescribe a bad diet. However, sometimes a little help is needed. At the CureCenter, we will prescribe medications and/or supplements that best suit your needs and lifestyle. Supplements that are most helpful include Bergamot BPF, Vitamin D3/K2, cinnamon, ALA and others.
I’m often asked about metformin. Metformin reduces glucose primarily by reducing release of glucose from liver stores of glycogen, but it is also considered a mild insulin sensitizer. There is a lot of interest in it as an antiaging and anticancer treatment. Its impact on cardiovascular outcomes is not as impressive as pioglitazone, a thiazolidinedione medication.
Pioglitazone improves insulin sensitivity. It is generic and has been around for a long time. It suffers from a bad reputation for fluid retention because its use was delayed till patients with Type 2 Diabetes had failed 1st line drugs that increased the risk of heart damage from prior heart attacks. But when used in the prediabetes stage, before the damage to the heart, it is generally well tolerated and dramatically reduces the risk of heart attack (>70% reduction) while lowering insulin levels. See Figure 3:
What is a Carotid Intima Media Thickness (CIMT) Ultrasound?
As part of your CurePlan, you will likely be asked to get a Carotid Intima Media Thickness (CIMT) ultrasound. This is different from the ultrasound done during our CureScreen process or the ultrasound you can get at your hospital or vascular specialist…
As part of your CUREPlan, you will be urged to get a Carotid Intima Media Thickness (CIMT) ultrasound if possible. This is more detailed than the CUREScreen carotid ultrasound process, carotid duplex ultrasound you can get at your hospital or vascular specialist or Lifeline Screening. It focuses your artery wall rather than the lumen and measures arterial inflammation, which is the measurable and reversible underlying condition of interest.
Lifeline screening identifies and encourages “monitoring” of plaque, but does not report intima media thickness for monitoring or offer a plan other than referral for surgery for late stage disease. It is useful for screening but not monitoring or proactive early intervention. If you have had a Discover Scan ultrasound, you already have more information then a Lifeline Screening ultrasound will offer, making it a waste of time and money better spent on a Carotid Intima Media Thickness ultrasound for disease monitoring.
CIMT measures the thickness/inflammation of the artery wall and documents the characteristic or stage of of plaque. It is typically repeated every 6-12 months measuring the artery wall thickness. Trained scanners with Butterfly ultrasound probes can provide images sufficient for CIMT reports, increasing convenience and availability.
A thicker wall is a sicker more inflamed wall with a higher risk of developing new unstable plaque. This inflammation triggered by injury and oxidative stress from many sources sets the stage for plaque development and rupture, the event leading to stroke, heart attack, dementia, erectile dysfunction, kidney failure, or other serious complications.
Having a little bit of arterial disease is like having a little bit of cancer. Like early cancer detection, our goal is to reverse arterial disease and achieve durable remission. When remission is prolonged and stable, we think of it as cured. CIMT offers the most cost-effective, painless way to monitor progress toward a cure for arterial disease.
What is the difference between a CIMT and a duplex carotid ultrasound?
The CIMT offers more meaningful information about early arterial disease than standard duplex carotid ultrasound. It documents the type of plaque (estimating risk of rupture) and measures the thickness/inflammation of the artery wall.
The purpose of the duplex carotid ultrasound is to determine the need for a surgical procedure by detecting late-stage disease while watching reversible early disease progress. Additionally, if you get a duplex ultrasound, your insurance likely won’t pay for the more informative CIMT exam for at least six months. Many vascular labs mistakenly or misleadingly answer “yes” when asked if their ultrasound is a CIMT. The best bet is to go with one of the 2 providers nationwide that offer reliable and consistent CIMT testing at locations and times around the country: Vasolabs and Cardiorisk.
At the CURECenter, we depend upon the CIMT because it allows us to detect reversible early disease, assign an “arterial age,” and show your improvement – something the duplex carotid ultrasound doesn’t do. This added information and ability to track your progress will motivate your journey to optimize your CUREPlan and reduce your burden of chronic disease.
A new process enables measurement of CIMT based on scans obtained by medical, dental and other professionals using point of care ultrasound supported by CURECoach, the Butterfly iQ ultrasound device and Vasolabs. Ask your dentist or doctor to consider this lifesaving opportunity for addition to their skill set and services.
What is arterial age?
The health of your carotid arteries reflects the health of arteries throughout your body - including the coronary arteries that supply blood to the heart. The carotid arteries are an accessible sample of a massive supply system.
Thickness, which is a reflection of sickness or inflammation, of your artery wall is compared to other people your age and gender as a population percentile. Your “arterial age” is the age for which the thickness of your arteries would be average, i.e. 50th percentile. At the CURECenter, we monitor arterial age every 6-12 months to ensure our plan is working and your arterial age is improving. It is like looking in the rearview mirror at inflammation for the past months. If it is not improving, we look for additional opportunities to improve your CUREPlan.
Does Insurance Cover CIMT?
Medicare covers carotid ultrasound AFTER a stroke or TIA. Most insurance covers CIMT if arterial disease is documented and measured. It is now possible to provide equivalent relevant information using Butterfly point of care ultrasound in the hands of doctors, dentists, and others. This makes it more available at more times in more places. It is more than sufficient to detect disease and measure regression/improvement. The cost is $198, making it an affordable out of pocket expense compared to the cost of disability and death.
Get Started on the Path to a Long and Healthy Life
Participate in a 15-30 minute Zoom or phone call with Dr. Backs. Your questions about process, cost, insurance coverage and expectations will be answered. You will decide together if the CureCenter and a CurePlan are right for you.
Located in Central Illinois? Schedule your 15-minute CureScreen for arterial disease. It’s quick, painless, and is the first step toward preventing the most common cause of death and disability.