CURE FAQs: Frequently Asked Questions
Answers to commonly asked arterial and metabolic disease questions.
Categories
Click on one of the categories below or type a keyword into the search bar to get started.
Recent FAQs
What is atherosclerosis?
Atherosclerosis is damage of the artery wall due to inflammation. Healthy arteries are important because they carry oxygen-rich blood from the heart to the entire body’s tissue and organs…
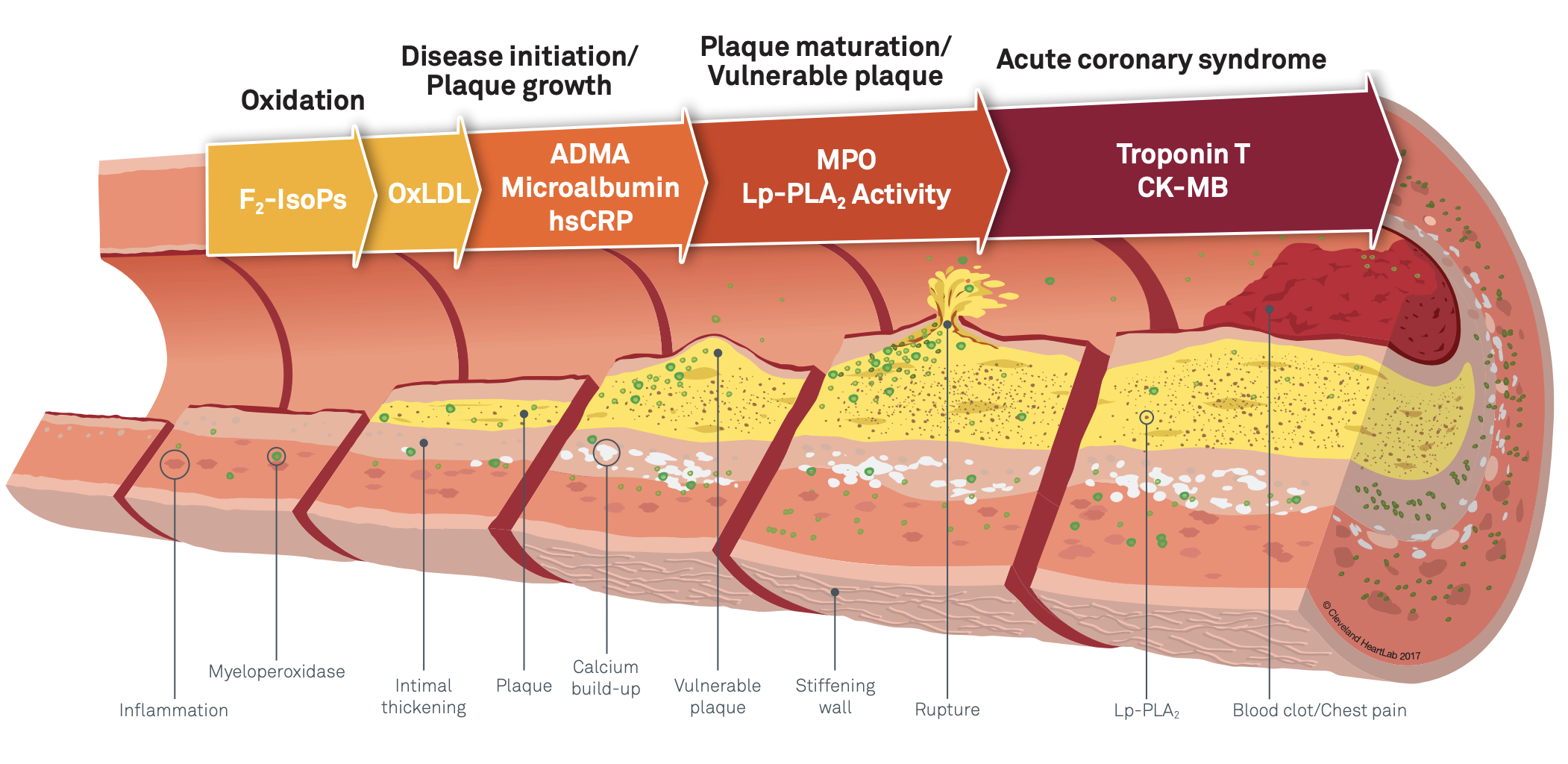
Atherosclerosis is Progressive but Reversible injury and inflammation of the artery wall. Healthy arteries are important because they carry oxygen-rich blood from the heart to the entire body’s tissue and organs. A more accurate description of the most dangerous stage of disease would be “atheritis” or “arteritis” meaning inflammation of the arteries. “Sclerosis” or hardening/calcification is a more benign later healed benign stage of the disease.
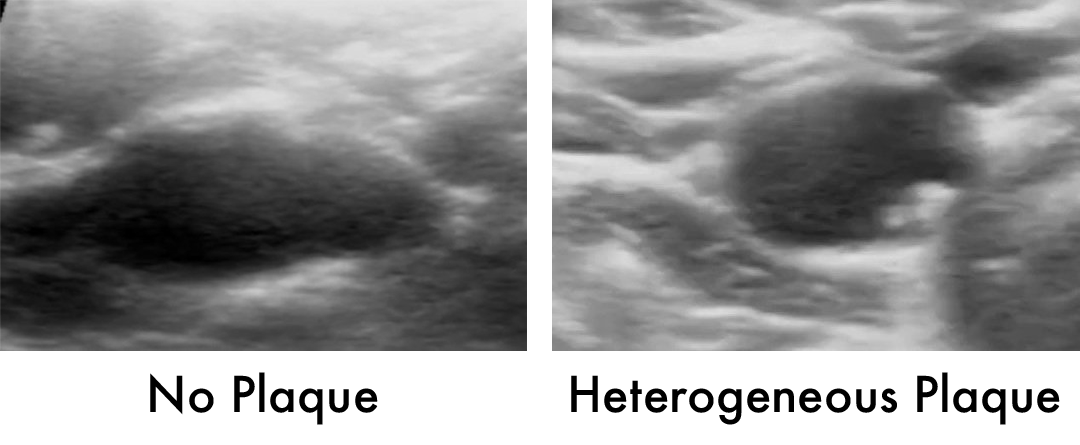
Acne is a relevant analogy most of us know. Inflammation in the skin (artery wall) creates pimples/plaque (in areas where turbulence adds mechanical shearing forces) that are prone to rupture (homogeneous and heterogeneous plaque) when new. The preferred path is to heal and leave a scar. When plaque is becoming calcified, it is healing. Rising coronary calcium score is a good, not bad, trend if you are on a healing program.
Atherosclerosis is often called “hardening of the arteries” due to a buildup of calcium deposits in plaque that forms in the arteries. However, calcium presence is actually a sign of healing and increases over time with new plaque development (bad) and current plaque calcifying (good). Plaque that has little or no calcium is less stable, more prone to rupture, and more threatening.
When your artery walls thicken with plaque and narrow the lumen, blood flow to any organ can be reduced or interrupted, leading to disability (temporary or permanent) or death. Stress tests and angiograms are useful to detect this phenomenon. However, the greatest danger is sudden plaque rupture and blood clot formation, resulting in heart attack or stroke. The best test to evaluate this stage is ultrasound for the carotid arteries (affordable) and AI processed coronary artery CT (expensive).
Source: Cleveland Heart Lab
How are arteries important to your health?
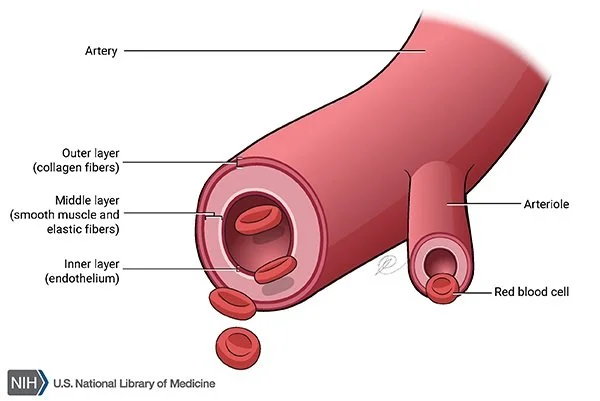
The heart pumps blood into the aorta and arteries, which then branch out into smaller blood vessels, eventually delivering the oxygen and nutrients to individual cells. Without healthy arteries, the body's tissues and organs would not receive the oxygen and nutrients needed to function properly. Maintaining healthy arteries is crucial for overall health and wellbeing. Arterial health improvement is a great reflection of reduced oxidate stress, inflammation and overall health improvement.
The artery wall has three layers:
Adventitia (outer layer): composed of connective tissue that supports and protects the artery from external injury.
Media (middle layer): made of smooth muscle and elastic fibers. It is responsible for regulating the diameter of the artery, which affects blood pressure and blood flow.
Intima (inner layer): a thin layer of endothelial cells that regulate all kinds of activity, maintaining a smooth surface for blood to flow through.
Image Source: NIH U.S. National Library of Medicine
What causes plaque to develop in the arteries?
Plaque grows due to complicated interactions between genetics, high blood pressure, lipids, inflammation driven by oxidative stress and insulin resistance, diabetes, and other conditions. Arterial disease is like acne and plaque is like a pimple or pustule.
Plaque progresses as follows:
Homogeneous plaque: This fresh, soft vulnerable plaque is like a new pimple. It is the most dangerous stage of plaque evolution because it is most likely to rupture and cause a heart attack or stroke.
Heterogeneous plaque: This type of plaque is like a pimple that is healing. It can still rupture or erode because inflammation has not resolved. It is the most common stage of plaque seen on imaging of arteries. It is an uneven buildup of inflammatory material, fibrin, and calcium.
Calcified Plaque: This type of plaque is the scar that results when plaque heals. Like any scar, we carry it for the rest of our lives but it is no longer a threat. Calcified plaque is the residual scar of a rupture-related event that could have happened, but didn’t! Calcified plaque is less likely to rupture, but can still cause problems by narrowing the artery and restricting blood flow.
As plaque is developing, it is vulnerable to rupture. A clot forms in the artery lumen. If the clot blocks an artery feeding your heart, you experience a heart attack. If it blocks an artery feeding your brain, you experience a stroke. Both can result in death or disability, but they can also be prevented by making artery walls thinner/less inflamed and healthier.
Atherosclerosis and its progression is more common but not inevitable as we age. Most adults have it starting in the thirties.
Using new science, testing, and treatments, we can halt and reverse the disease in our arteries.
Take the first step to prevent heart attack and stroke. Request a complementary Discovery Zoom Call with Dr. Backs and begin your journey to prevention and a healthy, happy life.
What are some red flags for arterial and other chronic diseases?
There are many conditions associated with arterial and other chronic diseases that lurk silently only to become suddenly lethal. These “red flags” reveal increased risk of heart attack, stroke, and other consequences of chronic disease…
There are many conditions associated with arterial and other chronic diseases that lurk silently only to become suddenly lethal. These “red flags” reveal increased risk of heart attack, stroke, and other consequences of chronic disease. They are not clearly causative or modifiable. But they can motivate curiosity and motivate.
Pay attention to them. The more red flags you recognize, the more you should want to know what may be lurking in you that could suddenly or slowly cost you your health… or even your life.
In addition to the following red flags, keep in mind that men over 40 years of age, women over 50, and individuals of African-American or Hispanic descent are also at higher risk of chronic disease.
Personal or family history of cardiovascular/arterial disease, heart attack, stroke, or Type 2 Diabetes
Age (men over 40 and women over 50)
Gestational diabetes
Elevated cholesterol
Nicotine use in any form (including second-hand smoke)
Psychosocial issues such as depression, anxiety, or stress
High blood pressure
Abdominal obesity (high levels of visceral fat)
Sleep problems (not enough sleep, sleep apnea, etc.)
Periodontal/Endodontal disease
Erectile dysfunction
Rheumatoid arthritis
Lupus
Psoriasis
Migraine headaches
Gout
Polycystic ovaries
Hirsutism (facial hair growth in women)
Osteoporosis
Pre-eclampsia
Breast cancer treatment
COVID spike protein infection or injection
If you fall into any of these categories, take the first step to good health and prevention, and request a complimentary Discovery Zoom Call with Dr. Backs.
How does Vitamin D Deficiency affect my health?
Vitamin D is an important nutrient that helps the body absorb calcium, which is essential for maintaining strong bones and teeth…
Vitamin D is an important nutrient, actually a hormone, that helps the body absorb calcium, which is essential for maintaining strong bones and teeth. It also plays a role in the immune system, muscle function, and reduction of inflammation. Optimal levels of vitamin D: 60-90 mg/dl. Don’t let anyone convince you that this can be “too high” and to stop your supplement. They don’t know the benefits of vitamin D levels above the population normal because the population as a whole is deficient.
Up to 75% of Americans are affected by suboptimal (< 50 ng/ml) vitamin D, which significantly increases the risk of heart attack, stroke, hypertension, diabetes, cognitive impairment, and cancer. Having darker skin, being obese, and not getting enough sun exposure to the skin are all linked to reduced vitamin D3 levels.
Symptoms of vitamin D deficiency include muscle pain, tiredness, fatigue, hair loss, back pain, bone loss, poor wound healing, and depression. It increases the risk of statin muscle pain. However, most individuals who are vitamin D deficient have no specific symptoms.
What causes vitamin D deficiency?
Inadequate sun exposure. Sunlight is the optimal source of vitamin D. When the skin is exposed to UVB radiation from sunlight, it produces a form of vitamin D known as cholecalciferol, or vitamin D3. Vitamin D3 is then converted into its active form in the liver and kidneys. This particularly affects individuals who are in institutions like nursing homes.
Dark skin. Melanin, the pigment that gives skin its color, reduces the skin's ability to produce vitamin D in response to sunlight. Melanin absorbs UVB radiation from sunlight, which is needed for the skin to produce vitamin D. This means that people with darker skin require more sun exposure to produce the same amount of vitamin D as people with lighter skin.
Old age. The skin's ability to produce vitamin D declines with age due to a variety of factors, including a reduced ability to convert sunlight to vitamin D, decreased skin thickness, and lower levels of the precursor molecules that are needed to produce vitamin D.
Obesity. Vitamin D is a fat-soluble vitamin, meaning it is stored in fatty tissues. Therefore, people with higher levels of body fat may require more vitamin D to achieve the same blood levels as people with lower levels of body fat.
Diseased kidneys. The kidneys are important for converting vitamin D into a form that the body can use. If the kidneys are not working well due to a disease, they may not be able to convert vitamin D properly, leading to a deficiency of vitamin D in the body.
Digestive tract issues (such as Crohn’s disease, celiac disease, or cystic fibrosis). Vitamin D is a fat-soluble vitamin, which means it needs to be absorbed in the presence of dietary fat in the small intestine. Digestive tract issues can affect the absorption of vitamin D in the small intestine. These conditions can cause inflammation or damage to the intestinal lining, which can interfere with the absorption of dietary fat and, consequently, vitamin D.
A vegan diet without proper supplementation. Vitamin D is primarily found in animal-based foods such as fatty fish, liver, and egg yolks. Therefore, people following a strict vegan diet that avoids all animal products are at risk of vitamin D deficiency.
Sunblock. When the skin is exposed to ultraviolet (UV) radiation, it triggers the synthesis of vitamin D3, which is then used by the body. However, using sunblock or sunscreen can reduce the skin's ability to produce vitamin D, as it blocks the UV radiation from penetrating the skin. It's important to find a balance between protecting your skin from harmful UV radiation and ensuring adequate vitamin D levels.
How can I treat vitamin D deficiency?
Increase sun exposure. Make an effort to get a healthy amount of sun exposure without putting yourself at risk for skin damage or skin cancer. It's recommended to get a moderate amount of sun exposure, typically around 10-15 minutes per day, without sunscreen, on the arms, legs, and face.
Eat vitamin D rich foods. Foods that are rich in vitamin D include salmon, sardines, tuna, egg yolks, fortified milk, and shiitake mushrooms.
Vitamin D supplements. Supplementation can bring your levels into the optimal range. We recommend a combination of Vitamin D3 and Vitamin K2. Vitamin K2 enhances vitamin D absorption, delivery, and the binding of Vitamin D3 in the appropriate tissues, enhancing its activity and benefit. Vitamin K2 also improves arterial elasticity and insulin sensitivity. The product we stock and recommend is called "K Force."
How do I know if I’ve properly treated my vitamin D deficiency?
Get a blood test measuring the serum concentration of 25(OH)D3. A “normal” level of vitamin D is at least 30 ng/mL or higher. However, our “optimal” range is 60-90 ng/ML.
If you have been diagnosed with vitamin D deficiency and have started taking supplements or made changes to your diet, get your vitamin D levels retested after a few months.
Get Started on the Path to a Long and Healthy Life
Participate in a 15-30 minute Zoom or phone call with Dr. Backs. Your questions about process, cost, insurance coverage and expectations will be answered. You will decide together if the CureCenter and a CurePlan are right for you.
Located in Central Illinois? Schedule your 15-minute CureScreen for arterial disease. It’s quick, painless, and is the first step toward preventing the most common cause of death and disability.